SHEA/IDSA/APIC 2022 C. diff Compendium: A Mighty, Brief Review

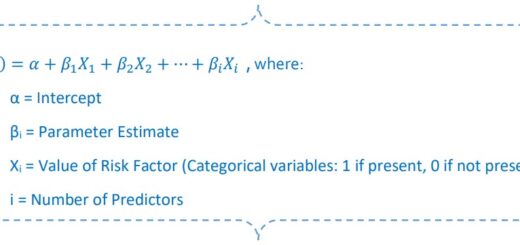
Depending on whether your laboratory uses a standalone or multi-step testing algorithm and depending on the test methodology(ies) used — and in which order — a positive C. diff test might be detecting colonization rather than infection.
Not good.
Here’s what the authors of the updated C. diff compendium have to say about antibiotic treatment for C. diff in the setting of a negative toxin immunoassay (EIA) test and a positive nucleic acid amplification test (NAAT):
“…data from the CDC (not yet published) suggest that >75% of patients are treated for CDI despite having a negative toxin EIA following a positive NAAT even though data suggest that treatment may not be necessary.”
Diagnosing C. diff Colonization Is a Problem
C. diff NAAT only detects the gene responsible for toxin production. It doesn’t detect the C. diff organism and it doesn’t detect actual toxin. NAAT testing, either standalone or the last of a multistep test algorithm, can lead to misdiagnosing colonization as CDI because the test cannot differentiate between colonization with a toxin-producing strain and actual toxin-induced disease.
Diagnosing C. diff colonization can lead to:
- Unnecessary antibiotic exposure.
- Unnecessary isolation precautions.
- Denial of a patient’s transfer out of the hospital to a lower level of care.
- Prolonged hospitalization.
These consequences affect the patient’s care experience and a hospital’s quality outcome measures.
To help home in on appropriate patient selection and C. diff test collection, we will review section 2, part 2: Identification of Patients with CDI and Appropriate Test Utilization from the SHEA/IDSA/APIC compendium, “Strategies to Prevent Clostridioides difficile Infections in Acute Care Hospitals: 2022 Update.”

Recommended Strategies to Improve Appropriate Testing Practices
Recommendations to improve identification of patients with CDI and C. diff test utilization include:
- Establish criteria for CDI test collection, processing and test interpretation regardless of the test method(s) used.
- If NAAT testing is used as part of a multistep algorithm, then facilities should establish specific treatment guidelines for patients with positive toxin EIA results versus positive NAAT results.
- Test patients with new onset, unexplained, clinically significant diarrhea.
- The compendium points out the possibility that a patient who’s on laxatives or new tube feeds can also have CDI. The decision to test/not test should be made after reviewing the timeline of diarrhea and associated symptom onset.
- Consider stool-inducing medications and other causes of diarrhea before ordering C. diff testing.
- Ask the provider to hold laxatives for a day or two to see if the diarrhea resolves. Most docs are agreeable to it in my experience.
- Avoid repeat testing during the same episode of diarrhea, or within 7 days of a previous positive test result.
- Avoid test of cure
- Toxigenic C. diff may be detectable in stool for weeks after the patient is successfully treated.
CDI Is a Clinical Diagnosis
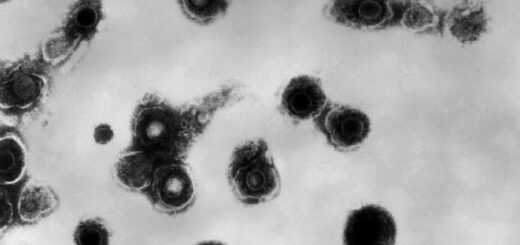
CDI is a diarrheal disease caused by overgrowth of a toxin-producing C. diff strain. It’s the toxins that cause the signs and symptoms of CDI.
The definition of clinical CDI with positive laboratory confirmation requires the patient has clinically significant diarrhea (with or without abdominal cramping) or toxic megacolon without a known cause. Specifically:
- New onset of a sustained change in stool consistency and/or frequency.
- The stool must be unformed and adhere to the shape of its container.
- Diarrhea is defined as at least 3 unformed stools in a 24-hour period.
The bottom line is new onset of unexplained diarrhea warrants C. diff testing.

Call to Action
Take some time to familiarize yourself with the compendium. If nothing else, review section 2.
The more you know about C. diff testing appropriateness the better you can educate your patients and advocate for them if you find they don’t fit testing criteria.
And equally important, feel confident when you collect and send a specimen for C. diff testing.