I Signed Up for This: An IP’s Journey Through a Candida auris Outbreak
Communicable disease transmission. It’s not a matter of if, it’s a matter of when because it’s only a matter of time. It happens in the best of medical centers.
I know because it happened in my medical center.
Candida auris transmission that spiraled into an outbreak.
Murphy’s Law
It was Friday, Nov. 11, 2022. At 4 p.m. I decided to log on to the data-mining system to check lab results.
Whaaat?? A positive Candida auris lab result? From a skin specimen?
Disbelief forced me into cognitive deliberation: “That’s not a screening swab. It says skin. This is from a fungal culture. This isn’t a screening test. It’s a clinical culture!”
It was the hospital’s third end-of-the-day Friday Candida auris result in four months. First in July, again in September and again in November. All occurring on units I covered.
The July and September cases taught my colleagues and I how to best use our existing technology to efficiently conduct a large-scale exposure investigation.
Have a Process to Follow
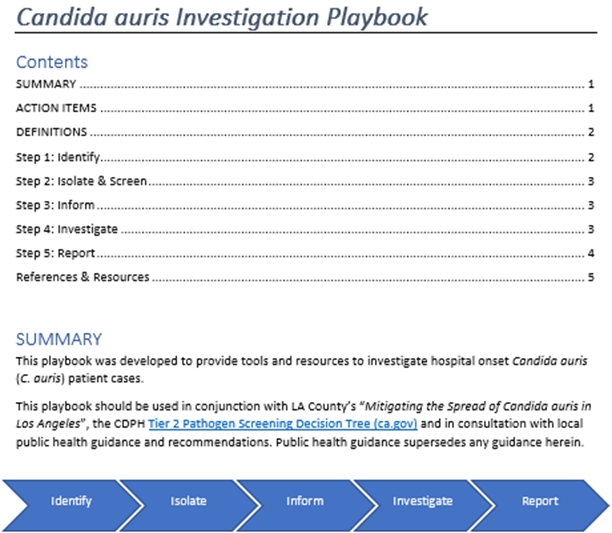
By November, it was more a matter of running the plays from our Candida auris investigation playbook. And while the plays are outlined, the work is still time-sensitive and labor-intensive.
“Outbreaks can just put the brakes on whatever you’re working on at the time,“ CloroxPro’s principal infection preventionist Doe Kley, told me. “That becomes your 100% focus.”
To complicate matters, the patient’s culture was collected Oct. 28, two weeks before the result posted.
Twenty-six days went by without isolation precautions (strike 1). I learned the patient was a direct admit from a skilled nursing facility; a high-risk admission that, per hospital policy, should have elicited an admission screening test, but didn’t (strike 2). And by hospital-day 19, the patient was suspected of having a fungal skin infection yet wasn’t placed in isolation (strike 3).
Self-doubt filled my head like smoke fills a room. Negative thoughts infiltrated my mind. I wondered if I rounded enough and if I educated enough. I felt like I failed somehow.
The playbook my colleagues put together is a refined product from the mad-dash exposure investigation we pulled off back in July.
Its structure follows the identify-isolate-inform strategy used in emergency departments for rapid assessment and management of patients with contagious diseases. It’s a step-by-step guide through the mud of an exposure investigation.
I Got By With a Lot of Help From My Friends
My teammates banded together to help me get through that late Friday afternoon investigation with what little time was left in the workday.
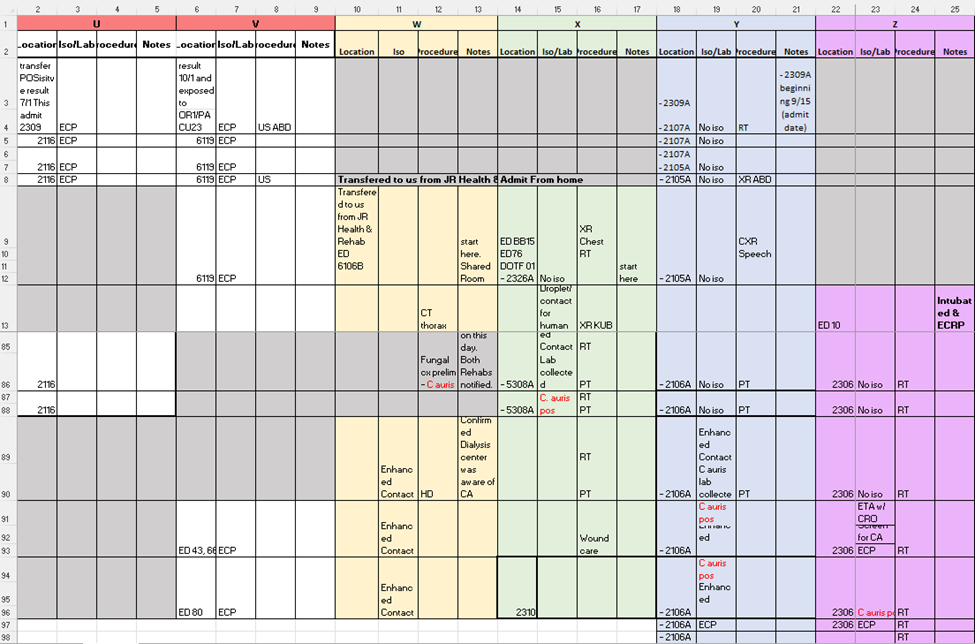
Contact tracing reports were pulled, reconciled, and those contacts still in the hospital identified. Roughly 35 potentially exposed patients were isolated and tested that night out of 150 contacts identified.
That was just the beginning.
By Nov. 16, we identified three more patients with Candida auris. They were identified one at a time, three days in a row. My confidence in infection control was waning.
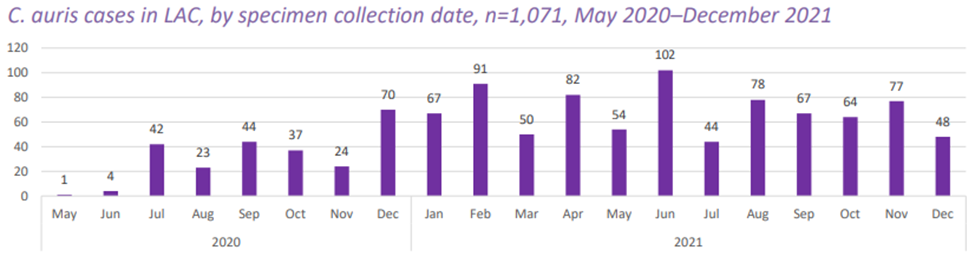
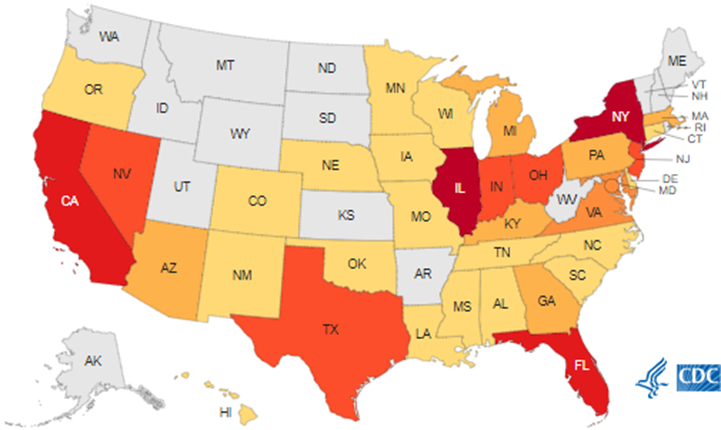
A remote haze still lingered from working in one of Los Angeles County’s hardest hit hospitals during the first and second waves of the COVID-19 pandemic.
We made the news for that.
Contact Tracing
I’ll refer to my Friday case as Mrs. W. She was discharged to another healthcare facility by the time her lab result posted. I notified both the transferring and receiving facilities.
Per mandate, we reported the case to California Department of Public Health’s Licensing and Certification branch and L.A. County’s Acute Communicable Disease Control program. ACDC knows me well; I have consulted with them on the topic of Candida auris in the past.
Contact tracing from Mrs. W’s investigation yielded a positive contact, Mrs. X. When a positive contact is found, the contact tracing process is repeated.
In doing so, we found Mr. Y. That same day we found Mrs. Z due to routine screening.
With four cases in less than a week’s time, we identified 382 contacts.
Because of that, ACDC opened an ICAR, an infection control assessment and response plan; a euphemism for outbreak investigation.
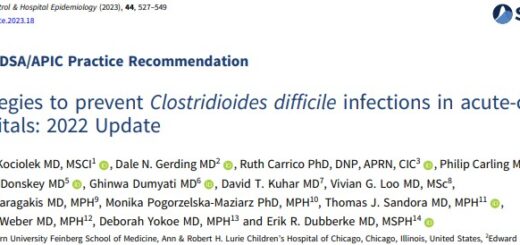
We had ongoing transmission and our epidemiologically linked contacts had overlapping stays on the same nursing units. ACDC recommended bi-weekly point prevalence surveys — screening every patient on specified nursing units at the same time – until no new positive patients were found.
Halleluiah
It took a lot of coordination between infection prevention, nursing and the laboratory, but we got the job done.
After five weeks of intense work and 1,000 swabs, ACDC closed their Candida auris outbreak investigation on Dec. 20, 2022.
We triumphed! We relished in relief. Six months later, I still feel a sense of relief.
During the height of the COVID-19 pandemic, I heard many healthcare workers lament they “didn’t sign up for this.” From time to time, I still hear it today.
I admit, I didn’t know exactly all I was signing up for when I decided to pursue infection prevention. Even though it sometimes feels like I signed up to clean messes, I know I signed up to help people, and I know I do.